Oct. 14, 2004 — In a pair of new studies, University of Utah scientists took early but significant steps to fight a particularly deadly childhood muscle cancer by identifying some of the genetic events that cause the disease and then engineering mice that develop the tumors. The genetic events might be targets for new drugs that could be tested on the mice.
The disease, named alveolar rhabdomyosarcoma, “is a very mean childhood cancer,” says study leader Mario Capecchi, co-chair of human genetics in the university’s School of Medicine and an investigator with the Howard Hughes Medical Institute. “Once the cancer has spread, 80 percent of the children are likely to die within five years, even with the most aggressive treatment possible, including chemotherapy, surgery and radiation.”
Capecchi says the studies provide evidence that the cancer may originate in mature or nearly mature skeletal muscle fibers. That is controversial because satellite stem cells – cells that become new muscle – long have been suspected of giving rise to rhabdomyosarcoma.
“If we know where it starts and the cause, you might be able to prevent it, detect it early or develop new treatments based on a better understanding of the biology of the tumor,” says Charles Keller, a pediatric cancer specialist and first author of the studies.
During the past 30 years, “there have been dramatic improvements in cure rates for a number of cancers,” he adds. “However, the outcome for advanced alveolar rhabdomyosarcoma has remained largely the same for 30 years.”
Until now, scientists have been unable to breed mice with alveolar rhabdomyosarcoma, so “we understand the initiation and progression of this disease very poorly,” Keller says. “This work represents a significant step forward in the understanding of the disease, and puts us on the path toward new therapies” less toxic to patients and better aimed at the cancer.
Keller and Capecchi believe it still will take 10 to 20 years for new treatments to emerge. But, Keller adds, “After 30 years of limited progress, we have our foot in the door.”
The new studies will be published Nov. 1 in the journal Genes & Development, with one of the studies published online Oct. 15. The studies involved mice, which have a genetic makeup quite similar to humans and thus are used as “models” for study of human diseases.
Co-authors of the studies were University of Utah undergraduate Mark Hansen; Cheryl Coffin, a physician in pediatric pathology; Benjamin Arenkiel, a graduate student in human genetics; and Harvard Medical School’s Nabeel El-Bardeesy and Ronald DePinho.
A Mutant Fusion Gene’s Role in Muscle Cancer
Childhood cancers are rare because cancer is primarily age-related. The American Cancer Society says that out of 1.37 million new cancers in the United States this year, 9,200 would occur in children age 14 or younger, and 313 of those would be rhabdomyosarcomas.
The American Cancer Society says 78 percent of children with cancer survive at least five years. But Keller says five-year survival is a dismal 5 percent to 30 percent – depending on the group studied – among children with alveolar rhabdomyosarcoma, the most severe form of the disease. (Another form, embryonal rhabdomyosarcoma, is more responsive to treatment.)
Capecchi says the cancer causes tumors in various muscles throughout the body, primarily in the legs, arms and shoulders, but also in the back, neck, trunk and even the tongue.
Scientists already knew that 85 to 90 percent of children with alveolar rhabdomyosarcoma have an oncogene – a cancer-causing gene – named Pax3:Fkhr.
It is known as a “fusion gene” because it forms when two chromosomes each break into two pieces and then fuse or recombine. The fusion gene includes a piece of Pax3 – which plays a role in forming the muscles, nervous system and head – and piece of Forkhead of Fkhr, a gene that acts as a tumor suppressor to control cell division, which runs amok in cancer. Researchers believe Pax3:Fkhr causes cancer by triggering inappropriate muscle development.
Unraveling the Workings of a Cancer Gene
In their first study, the researchers probed how the Pax3:Fkhr fusion gene affected development of the mouse embryo, muscle formation in the embryo, and muscle growth that occurs after the mouse is born and satellite stem cells give rise to new muscle cells.
They engineered a version of the Pax3 gene that could be converted into a Pax3-Fkhr fusion gene at any stage of embryo development and in any desired cells – a new technology called “conditional mutagenesis.” Capecchi says these experiments revealed how the fusion gene turns various genes on or off, interfering with normal muscle development and providing clues to the complex series of steps by which the gene causes alveolar rhabdomyosarcoma.
“If you know the steps involved, then you can look at each of them and ask, ‘Are there drugs that would specifically interfere with that step,'” he adds.
Keller says muscles are made two ways. As an embryo grows, muscles develop from cells known as somites, which also give rise to bone and skin. Just before birth, muscle starts being made a second way: Muscles made earlier gain added mass because of satellite cells, which are stem cells destined to make muscle.
Rhabdomyosarcomas long were thought to arise in satellite stem cells. Yet when the researchers activated the cancer-causing Pax3:Fkhr gene in mouse muscle satellite stem cells, the embryos didn’t develop tumors. That makes satellite cells an unlikely source of the cancer.
Scientists who reviewed the paper argued the cancer could still originate in rare subtypes of muscle stem cells. Keller and Capecchi plan to test those cells. But Keller says that when the Pax3:Fkhr fusion gene was turned on in tens of thousands of satellite stem cells, those cells didn’t become cancerous, so it seems likely the gene must cause cancer by becoming active in some other type of cell.
In the second study’s key finding, mice developed muscle tumors much like the human cancer when Capecchi and Keller did two things. First, they activated the Pax3:Fkhr cancer gene in mature or nearly mature muscle fibers either late in development of mouse embryos or after the mice were born. Second, they inactivated either one of two tumor-suppressor genes – named Trp53 (or p53) and Ink4a/ARF – that normally control cell division.
Recent experiments show nearly all the mice develop muscle cancer when the scientists activate the Pax3:Fkhr cancer gene and deactivate either tumor suppressor gene, Keller says.
Mice previously have been created to develop the less deadly embryonal rhabdomyosarcoma muscle cancer, and a rare type, known as pleomorphic rhabdomyosarcoma, but until now, no mouse had developed the highly lethal alveolar rhabdomyosarcoma.
Capecchi says cancer specialists have believed alveolar rhabdomyosarcoma originates in satellite stem cells because the tumors proliferate after birth, when stem cells retain their ability to proliferate but mature muscle fibers normally do not. Also, a number of cancers involve stem cells. So “it’s a big deal for a [mature or nearly mature muscle] cell not be proliferating and then all of a sudden to be able to proliferate” to form tumors, Capecchi adds.
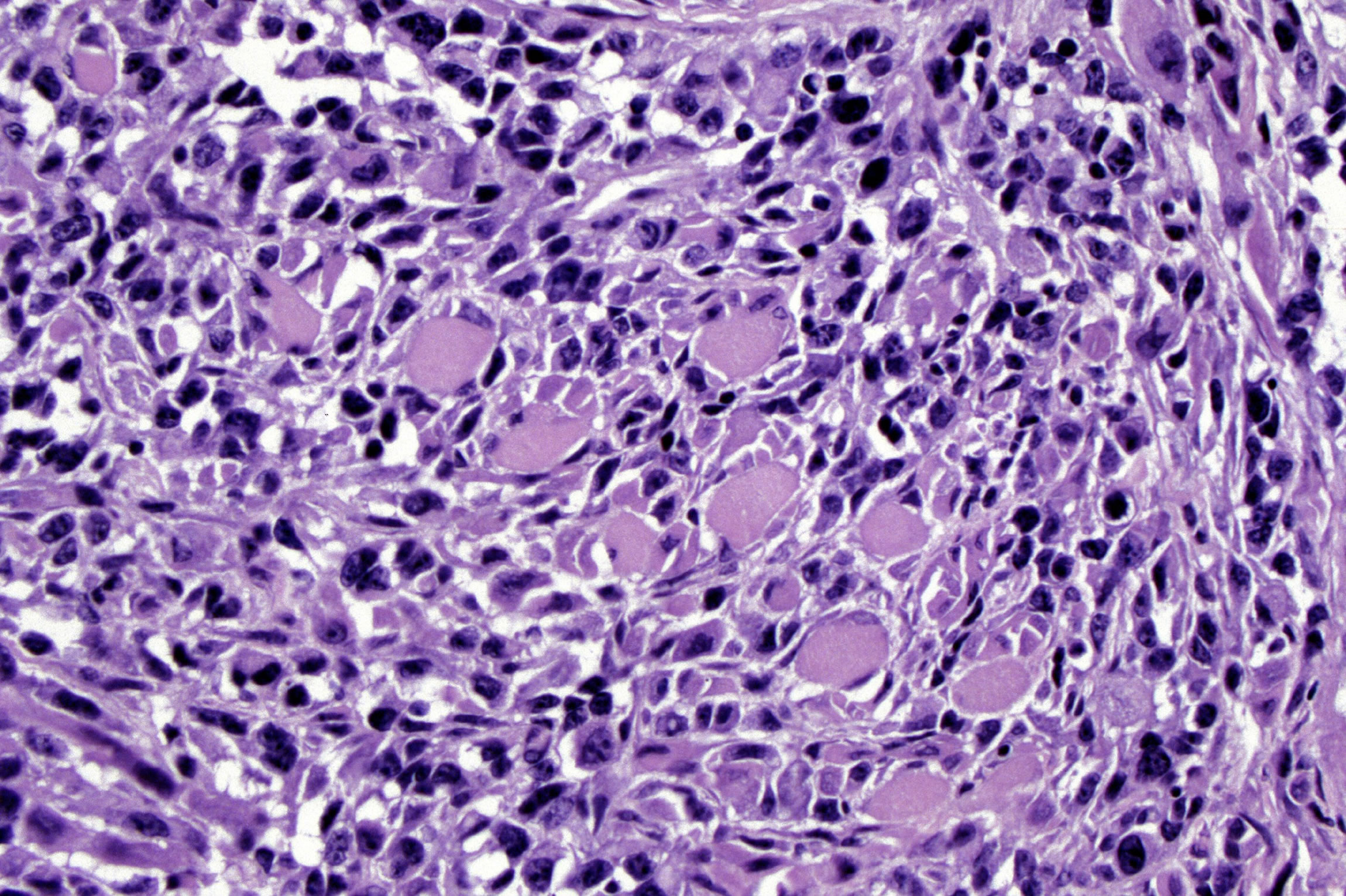
Keller says other researchers previously found that maturing skeletal muscle cells grown in the laboratory can revert to muscle stem cells. The Utah research found that tumors arising from mature or nearly mature muscle in mice have some characteristics of stem cells. That suggests the “primitive-appearing [rhabdomyosarcoma] tumors may be the result of non-primitive [muscle] cells reverting to a primitive state,” Keller says.
Mice with rhabdomyosarcoma now can be studied to determine how the cancer arises from mature or nearly mature muscle fibers, and also whether the Pax3:Fkhr fusion gene is required to maintain the cancer or just to get it started.
